Aim
To review all medico-legal claims finalised nationally pertaining to Emergency Medicine during 2014 and identify learning opportunities. A finalised claim is one in which all the financials have been agreed, but not necessarily paid.
Method
A retrospective one year review of all claims finalised nationally in Emergency Medicine in 2014, pertaining to adults, was conducted. This list was obtained using the NIMS (National Incident Management System) and a data search performed using the term ‘Emergency Medicine’.
Results
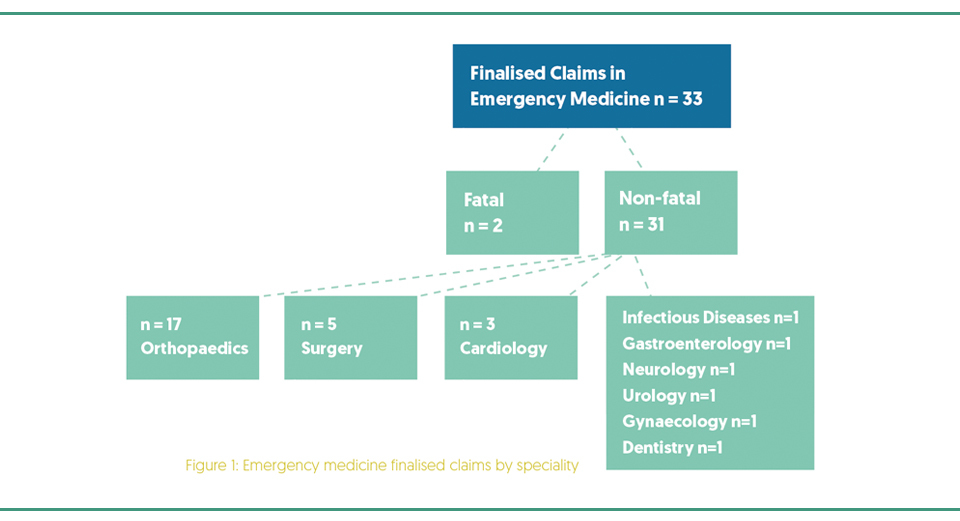
Fifty six finalised claims were identified, of which 23 (41.1%) were excluded: 10 were statute barred, 6 were withdrawn by the claimant, 3 pertained to paediatric emergency medicine and 4 were miscategorised. Of the 33 (58.9%) finalised claims, 20 (60.6%) related to male patients.
Two claims (6.1%) resulted in fatalities. One pertained to a patient with no known drug allergies, who developed anaphylaxis: adrenaline was not administered. The second related to a patient who was discharged from the Emergency Department (ED) with gastritis and collapsed at home. Despite resuscitative efforts, the patient died secondary to a perforated duodenal ulcer.
With regard to the non-fatal claims (Figure 1), multiple specialities were identified, of which orthopaedics (n=17, 54.8%) was the most common, followed by surgery (n=5, 16.2%) and cardiology (n=3, 9.7%). There was one (3.2%) claim each in the specialities of infectious diseases, gastroenterology, urology, neurology, gynaecology and dentistry.
Regarding orthopaedics (n=17), delayed diagnosis of fracture (n=9), was the most common claim; followed by unexpected complication after treatment (n=3) which included infection (n=2) and nerve damage (n=1). The remaining orthopaedic claims involved missed septic arthritis (n=2), cauda equina (n=1), finger injury (n=1) and wrong limb x-rayed (n=1).
Surgery accounted for five claims, of which three related to delayed diagnosis of appendicitis. An emergency laparotomy for acute peritonitis secondary to a perforated and gangrenous appendix was required in one case. The patient had presented two days earlier with abdominal pain, vomiting and diarrhoea and a diagnosis of gastritis had been made.
Cardiology claims (n=3) pertained to a delayed diagnosis of non-ST elevation myocardial infarction; a retro-peritoneal clot post angiogram and a suboptimal cardiopulmonary resuscitation where defibrillation was repeatedly impeded due to excessive chest hair.
The single Infectious Disease claim resulted from a high risk patient who presented with varicella infection on a background of immunosuppression secondary to an organ transplant. A delay in commencement of treatment resulted in acute renal failure and a cerebrovascular accident.
A breakdown of claims by incident type identified that “delay in diagnosis” was the most common (n=23, 69.7%), followed by “delay in treatment” (n=4, 12.1%) and “unexpected complication of treatment” (n=6, 18.1%).
69.7% of claims due to delay of diagnosis.
12.1% of claims due to delay of treatment.
Lessons learned
- Implement specific Education and Training in clinical and radiological presentations of orthopaedic cases prior to commencement of ED rotation.
- Recognition of high risk patients with appropriate referral and escalation to senior decision makers.
- Importance of clear, accurate and timely documentation. Poor quality documentation is a criticism in many expert reports and HSE and HIQA investigations (HSE, 2014; HIQA, 2013).
*Data validated as of the 13/05/2015
Article by: Fiona Culkin and Deirdre Walsh, Clinical Risk Advisers, State Claims Agency
References available on request




