In this article, Dr Karen Power, Clinical Risk Researcher, outlines learning from catastrophic claims relating to babies in maternity services and presents advice to assist frontline staff in mitigating the risk of these claims occurring.
A range of indicators, including perinatal mortality rates1 and maternity mortality rates2, point to the safety of maternity services in Ireland. However, claims arising from catastrophic injuries to babies in maternity services account for more than half of the State’s total outstanding liability from claims and more than two-thirds of the State’s outstanding liability in respect of clinical claims.
The State Claims Agency (SCA) recently completed a five-year review of claims arising from catastrophic injuries to babies in maternity services. The review included claims involving injuries to babies before or during labour, or up to 28 days postnatally. Of the 80 claims reviewed, 74 arose from incidents occurring before or during labour and this article focuses on the features of those claims.
Features of the mother, labour and infant
Our review of these seventy-four claims showed that:
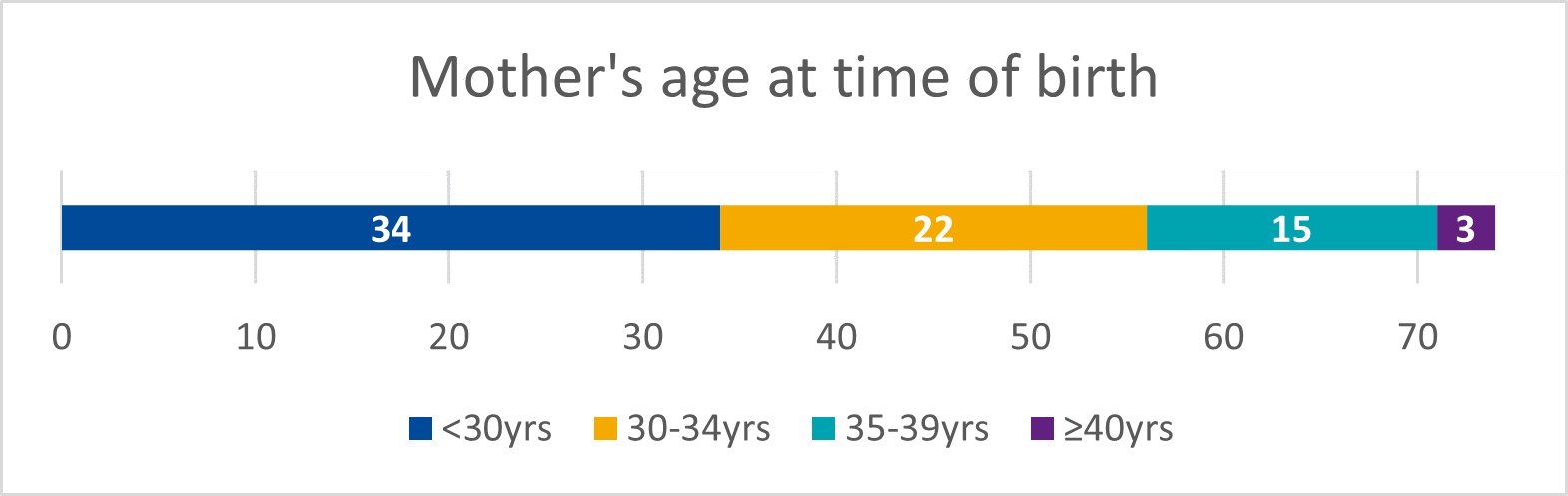
- 66% of women were nulliparous and 46% were under 30 years of age (Figure 1)
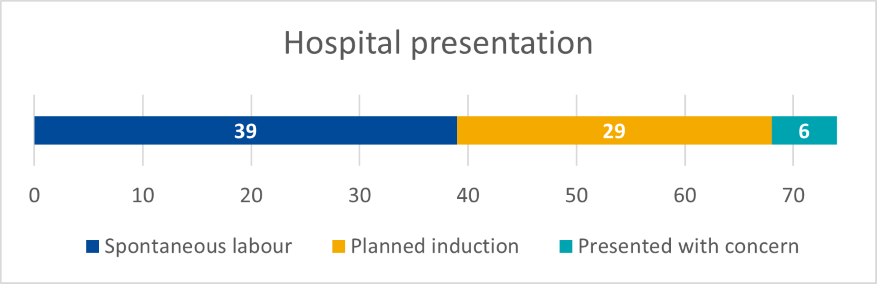
- 53% of women presented in spontaneous labour (Figure 2)
- 24% of labours involved an acute obstetric emergency
- 47% of babies were delivered by emergency caesarean section, which is higher than the national average (27-44% for 2021 data1)
- 30% were born by instrumental delivery
- 59% were male babies
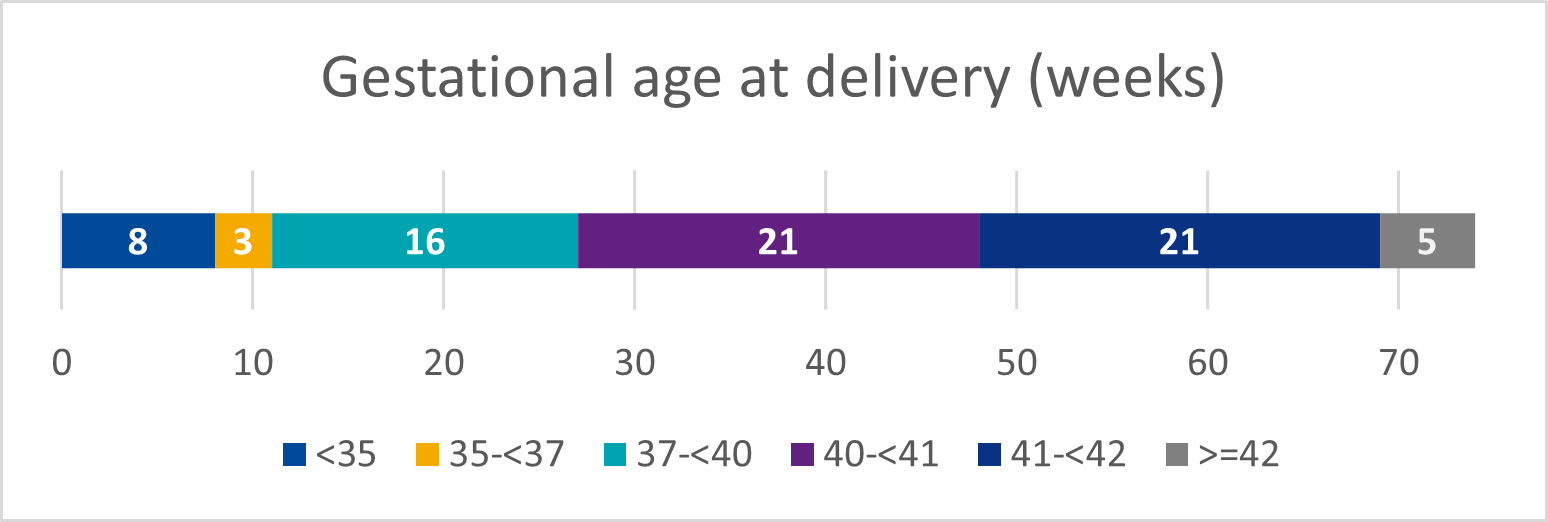
- 25% would be considered small for gestation age when weight and gestation were plotted on a standardised fetal growth chart (Figure 3).
Learning from claims
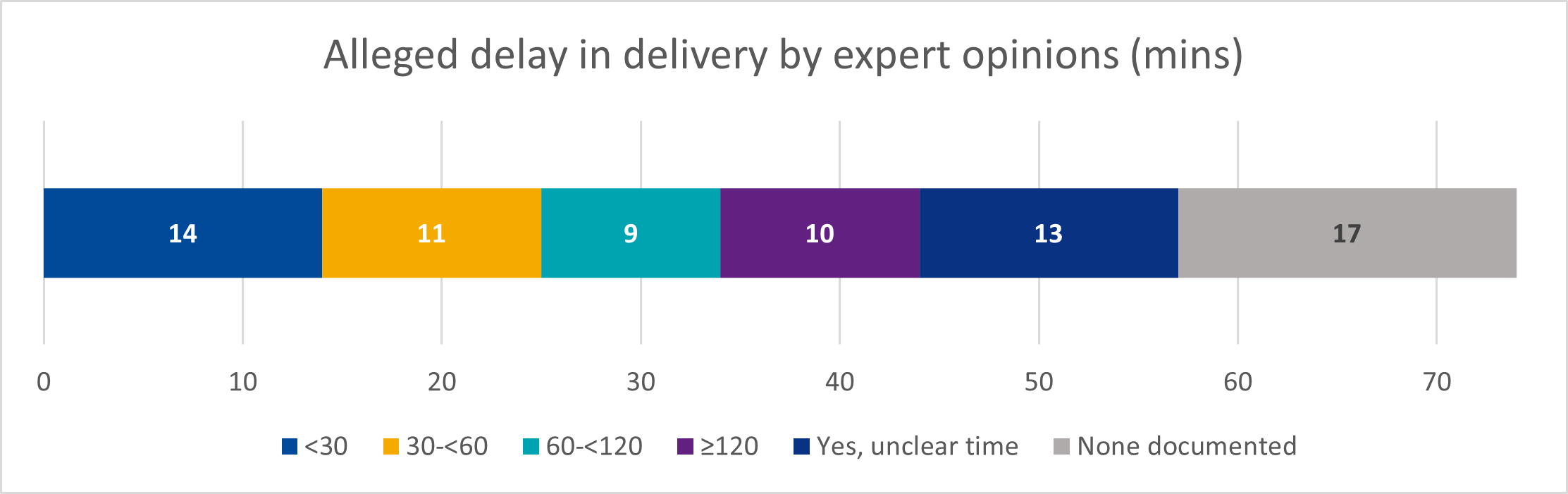
In 77% of the claims, there was evidence of a delay in delivery, with a delay of 30 minutes or greater in 58% of claims.
Specific issues identified in the claims included:
- Absent or poor-quality documentation, making defence of the claim difficult
- Failure to correctly interpret or recognise an abnormal or pathological CTG
- Failure to monitor fetal heart/uterine contractions appropriately
- Delay in escalation of clinical concerns to a senior decision-maker
- Inappropriate or incorrect use of oxytocin
- Inadequate examination or assessment of the mother
How can frontline staff mitigate the risks of such claims occurring?
Based on our analysis of these claims, we provide the following key advice for frontline staff:
- Recognise deviations from normal and ensure appropriate and timely intervention/decision-making when clinical concerns are present
- Ensure timely transfer to theatre when a decision is made for a caesarean section, based upon the assigned emergency category, and ensure that all relevant members of the multidisciplinary team are available
- Anticipate the need for multidisciplinary assistance (e.g. neonatal paediatrician, microbiologist) and communicate this as soon as possible to the relevant teams
- Recognise that the CTG should not be interpreted in isolation, but rather as part of a holistic assessment of fetal and maternal wellbeing
- Know when passive cooling and therapeutic hypothermia is indicated/appropriate and ensure prompt referral to a specialist centre, where indicated
- Escalate concerns regarding fetal and maternal wellbeing to the senior midwife and obstetrician without delay
- Consider a "fresh eyes and ears" approach to fetal monitoring; have a colleague perform a fresh review of the fetal heart rate during intermittent or continuous fetal monitoring, and document that review with time and signature
- Know when oxytocin is indicated/contraindicated and the appropriate dose and method of administration for the different clinical scenarios in which it is used
- Know when and how to perform additional examinations for suspected intrauterine growth restriction (IUGR)
- Ensure documentation is of a high standard by maintaining legible, complete and contemporaneous notes. Ensure the CTG record is complete and that it includes a record of fetal heart rate, tocograph, accurate date and time, and maternal pulse
- Maintain your skills by undertaking regular education and skills and drills training on fetal monitoring and the management of obstetric emergencies
References available upon request.
For more, see Claims Review Report: Catastrophic Claims relating to Babies in Maternity Services.
Take our survey
If you have a moment to spare, would you be willing to answer a few questions? We’d greatly appreciate your feedback. Our short survey will take about 5 minutes. Thanks for your help.
Clinical Risk Insights
View more articles from the latest edition of Clinical Risk Insights by the State Claims Agency.








